Recently, I enjoyed a vacation to the Outer Banks of North Carolina and was reflecting on my earlier years of onboarding new coders. Often, the first records that were assigned consisted of obstetrics (OB) and newborns. What was I thinking? How did I ever believe that coding up to nine months of conditions impacting the miracle of childbirth could be simple? Experience has taught me that change can be a good thing, as evidenced by ensuring new and seasoned coders receive the instruction needed to code OB charts correctly.
October 1, 2015, brought about some of the most important, yet challenging coding concepts with the implementation of ICD-10 CM (clinical modification) and PCS (procedure coding system). OB diagnosis coding moved from an episode of care to a trimester and weeks of gestation axis. Chapter 15 codes retain their sequencing priority status over other condition codes unless the provider documents otherwise. Obstetrics codes are all assigned with alphanumeric codes beginning with the letter “O” making the recall and recognition of OB codes familiar for coders and data analysts. It is inaccurate to assign OB codes for the newborn record.
Often confusing for coders is the assignment of the final character of the trimester. ICD-10 CM has specific timelines that represent the trimesters:
- First Trimester – less than 14 weeks 0 days
- Second Trimester – 14 weeks 0 days to less than 28 weeks 0 days
- Third Trimester – 28 weeks 0 days until delivery
Assignment of the trimester depends on the provider’s documentation of the trimester (or weeks of gestation) for the current hospital admission or encounter. Adding to the coding dilemma, there are conditions that occur in pregnancy that are linked to specific weeks of gestation. An example is hyperemesis gravidarum. A specific timeline for excessive vomiting in pregnancy is given as before or after 20 weeks of gestation. There is no reference to trimester, therefore, for accurate code assignment, the provider would have to provide weeks of gestation regardless of trimester documentation or a query would be needed.
High-risk patients often require admission to the hospital in one trimester and may remain an inpatient into another trimester. When this occurs, it is the trimester in which a condition occurs that is assigned as the final character. “If the condition developed prior to the current admission/encounter or represents a pre-existing condition, the trimester character for the trimester at the time of the admission/encounter should be assigned.”
One of the biggest opportunities in coding is Principal Diagnosis Selection (PDX). The driver of medical and surgical DRG’s is the PDX. The same is true when considering OB coding. The reason for admission after careful study still applies. The admission for vaginal delivery requires that the PDX relate to the main circumstances or complications of delivery. When we consider a patient admitted for cesarean delivery, the condition associated with the reason for the cesarean section is the PDX. If the OB patient requires admission for an unrelated condition, not associated with the delivery, and does delivery on this admission, the PDX is the reason for admission.
Upon presentation for delivery, the coder should read carefully for associated procedures being performed. When documented, consider:
Artificial rupture of membranes
Episiotomy
Epidural catheter placement
Forceps
Vacuum extraction
Vaginal delivery
Cesarean section
Laceration repair
Other
Depending on facility-specific guidelines one or more of these procedures may require PCS code assignment.
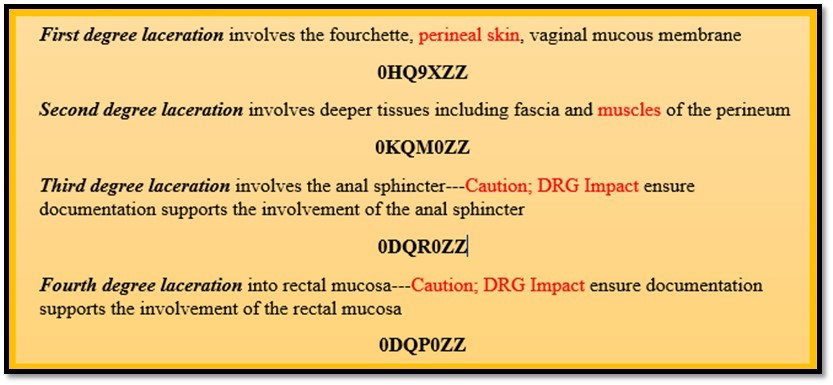
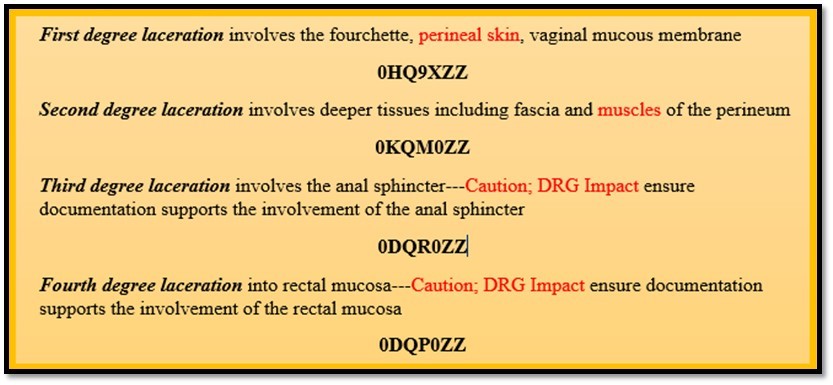
Perineal lacerations have been a recent topic of discussion among my coding colleagues. Inpatient coders are finding themselves questioning some of the DRG groupings when assigning OB laceration repairs. An understanding of issues involved in the OB laceration repair may shed some light on the subject. (See Figure below)
Additional potential DRG impacts include other obstetric lacerations involving the bladder, cervix, clitoris, urethral, peri-urethral, uterus, vagina, labia/vulva. Documentation is the key to correct code assignments. When grouping to the 98X DRG’s take a second look at the documentation and if there is any need for clarification, query the physician.
References: Official Coding Guidelines
About the Author
Marie Thomas holds a Masters in Healthcare Administration from Pfeiffer University, Charlotte, NC, and a Bachelor of Science in Healthcare Administration from Pfeiffer University. Marie has furthered her career education by becoming an AHIMA-Approved ICD-10-CM/PCS Trainer and Ambassador as well as earning the RHIT, CCS, CCDS, and CPC-H credentials. For more information please email us at contact@eclathealth.com