Achieving thorough and precise Clinical Documentation the first time sustains the Medical Coding quality driving the timely, optimal reimbursements that fuels both operations and strategic growth.
Even leveraging the most experienced Coding resources, gaps in clinical documentation inevitably cause revenue reductions and increased denials.
If you’ve identified gaps or suspect issues stemming from your Mid-Revenue Cycle are impeding returns and growth, a Medical RCM solutions partner like ECLAT Health Solutions will help you identify the appropriate solutions to best close them.
When gaps exist, issues arise. Documentation concerns can range from low diagnostic or procedural specificity, insufficient adherence to MEAT (Monitoring, Evaluating, Assessing/Addressing, Treating) criteria1 or undocumented medical necessity.2 Incorrect or incompliant documentation outlines a different medical encounter than occurred resulting in discrepancies in codes that can affect quality of care and reimbursement.
As the course of these issues through the revenue cycle continues, it becomes clear why we must address clinical foundations first. An incorrect medical record profile (or one not supported by the documentation) would be moved through the revenue cycle only to be denied.
Denied claims are costly. Reworking a single claim costs approximately $25.1 If we multiply this, the expenses of recurring denials quickly add up.
A third of denials made end up being unrecoverable,3 and denial rates have been increasing (typically between 6%-13%3 according to HFMA). Due to the time and experience required to rework claims, it has been estimated that 50% - 65% of claims are abandoned upon initial denial4 resulting in lost revenue. Even if you have ready access to the experienced Medical Coding services required, rework is always a drain on time and resources.
On the other side, since inaccurate or incomplete documentation is by nature not reflective of the entire medical encounter and all treatments and services rendered, it can leave behind revenue that is unsupported by the missed documentation.
While potential pitfalls abound, providers can best secure their mid-cycle by partnering with ECLAT Health Solutions. Pre-bill documentation, Coding quality/accuracy and revenue results can be improved leveraging our Mid-Revenue Cycle management resources and expertise.
Pre-Bill Clinical Documentation Improvement
CDI services focus on improving documentation accuracy and process efficiency for clean Coding that’s approved the first time. Refining documentation positively impacts revenue returns, but you can also reap tangible benefits before the cycle completes. Effective use of CDI results in
- Improved documentation to unburden physicians by reducing queries
- Reduced errors to free up resources invested in rework
These advantages not only contain costs but also condense the time required for the cycle to process the claim and return an accurate payout.
High-Quality Coding and Auditing
While evaluating Mid-Revenue Cycle performance, it’s important to consider the following questions.
- Are you consistently achieving optimal reimbursements?
- Do claims clear payer approval the first time?
- Are you experiencing recurring compliance issues?
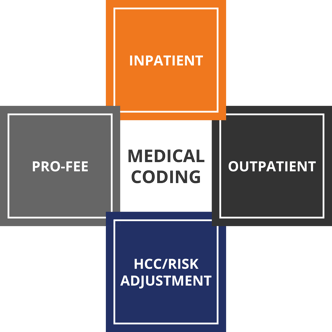
As we’ve seen, the high-quality coding required for optimal reimbursements is only achievable when documentation is correct and complete. Refined CDI solutions enable your Coding department to begin its work - whether Inpatient Coding, Outpatient Coding, Pro-Fee Coding or HCC/Risk Adjustment - with the most accurate and comprehensive outline of each patient encounter. Therefore, pre-bill documentation accuracy is one of every revenue cycle’s most vital priorities.
While many Coding issues can be resolved with CDI, Medical Coding solutions and resources remain vital to complete the chart efficiently and effectively. Common challenges include maintaining experienced resources in today’s competitive climate and ensuring sufficient education on all specialties you offer.
"The biggest hurdle RCMs continue to face is hiring and retaining the right resources with the appropriate skills", says VP, Revenue Cycle Operations, Marie A. Thomas, MHA, RHIT, CCS, CCDS. "ECLAT has the engaged, quality-driven CDI and Coding resources to achieve the optimal reimbursement."
Whether you need supplemental or outsourced assistance, an ECLAT partnership delivers high-quality revenue cycles results with certified, seasoned Coding resources that
- Significantly improve Medical Coding solutions quality with areas of concern
- Scale to any volume
- Expedite Coding processes to accelerate reimbursement cycles
- Maintain stringent compliance and security standards
Leveraging the right resources streamlines Medical Coding and Auditing processes to overcome issues with ease and accelerate reimbursements while containing costs.
Driving ROI with an RCM Partner
How can your revenue cycle derive the best results from a revenue cycle management solutions partnership and Medical Coding solutions provider? The answer depends on the partner you select.
A crucial consideration is your partner’s ability to leverage industrywide revenue cycle experience and specialty Coding resources at scale. Further, a unified combination of end-to-end solutions (CDI, Medical Coding, Medical Billing and A/R Management, Auditing) and technological assets will provide the right resources for any need, guiding each encounter from documentation through reimbursement.
Improved revenue returns, operational stability and broad strategic growth potential can be achieved by partnering with ECLAT Health Solutions. Leverage our certified, veteran Coding (Inpatient Coding, Outpatient Coding, Pro-Fee Coding and HCC/Risk Adjustment) and CDI resources as an extension of your team.
ECLAT empowers your health system to grow strategically and increase the resources/time available to invest in providing the best patient care possible. Let’s work together to resolve Mid-Cycle concerns and take your revenue cycle to new heights.
References:
- https://www.aapc.com/blog/41212-include-meat-in-your-risk-adjustment-documentation/ | AAPC
- https://acdis.org/articles/qa-defining-medical-necessity | ACDIS
- https://www.physicianspractice.com/view/why-getting-claims-right-first-time-cheaper-reworking-them | Physicians Practice
- https://www.mgma.com/resources/revenue-cycle/you-might-be-losing-thousands-of-dollars-per-month | MGMA



