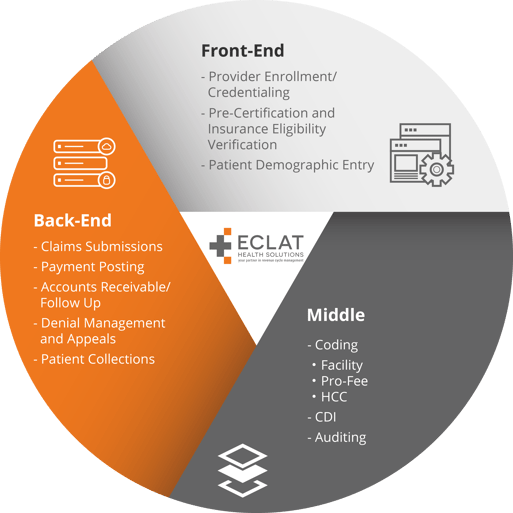
As defined by the Healthcare Financial Management Association1, revenue cycle refers to “all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” In short, it includes the entire lifecycle of a patient account, from initial appointment setup to payment receipt.
2020 presented challenges to the healthcare industry, not only in diagnosing and treating COVID-19 patients, but also in seeing the growth of telehealth services. A remote workforce, which had been common in other industries, became the norm for many healthcare workers who hadn't been doing remote work before. This was true for medical coders and other RCM workers.
While the ultimate aim of the healthcare practice is to deliver the best outcomes for the patients, this isn’t possible unless the administrative functions of a provider’s systems stable enough to handle revenue disruption.
With so many changes, it is not surprising that financial leaders at hospitals and health systems identified confusion over COVID-19 coding and claim requirements as one of the top issues impacting revenue cycle operations in 2020. Internal audits uncovered the average hospital claim denial rate increased during the height of COVID-19, hitting a new record of nearly 11 percent of claims denied upon initial submission in 20202.
Payment posting and collections are crucial indicators of a well-established revenue cycle management (RCM) system. Medical coding is the process of converting complex medical information, records, and documents to alphanumeric codes to simplify patient communications, billing, and revenue collection. In the era of value-based reimbursements, nothing plays a more critical role than having a team of experienced medical coding professionals aid in building a healthy revenue cycle and ensuring providers are correctly paid for the care they provide. Given that coding sits in the middle revenue cycle, providers often undermine its significance in ensuring each step before and after the coding process runs like a well-oiled machine. As an integral part of reimbursement in revenue cycle management, experienced quality coders are often the first to diagnose deficient pitfalls.
2021 continues to be another year of change. Historic changes to evaluation and management (E/M) coding took effect on January 1st and more than 60 new codes were added. Additionally, providers continue to see the need to have robust coding education and training in place to keep up with the COVID-19 code changes and prevent claim denials.
To uncover the vulnerabilities in today’s RCM, HIMSS Media surveyed3 100 respondents in leadership roles within finance, revenue cycle, reimbursement, and health information management. The results published established clinical documentation and coding as the key area of vulnerability for lost or decreased revenue - with 84% claiming this challenge as a “high” or “medium” risk.
When coding is done in the right manner, claims get processed quickly. On the other hand, missed deadlines, messy submissions, and lack of training often result in denied claims and cost your healthcare organization thousands of dollars in lost/delayed revenue.
Hospital revenue in 2021 is predicted to decrease between $53B to $122B compared to pre-pandemic levels because of COVID-19 says the American Medical Association.
So, the question is, how can Hospitals and health systems prevent dips in coding quality for a high-performing revenue cycle?
Revenue Cycle Management: Improve your coding quality for a high-performing revenue cycle
1. Pay attention to your EMR workflows.
The volume of charts to code is often so large and overwhelming that working denied claims takes a backburner.
Indeed, working denials is a cumbersome, time-consuming process that involves research, rework, and resubmission - all within a tight deadline.
Most importantly, it is essential to edit the practice management system and educate coders about the rules and regulations to prevent repeat errors.
Therefore, coding managers need to correct inefficiencies in the coding workflow to allow enough time for edits and reworks, which, if ignored, can slow down reimbursement.
Revisiting the coding workflow involves assessing if your coding department is adequately staffed to handle the workload, defining task list and priority, and deciding who will work on what part of the process (i.e., new claims, denials, and edits)
2. Partner with the best Medical Coding resources
Hiring high-quality coders is one of the best ways to improve RCM medical coding.
RCM leadership is tasked with –proper due diligence which includes the following verifications:
- Coders have certifications from accredited healthcare organizations, including AAPC and AHIMA.
- Coders are aware of their significant role in RCM, work proactively towards quality assurance, seek continuous education and training to keep abreast with changes in the healthcare environment, and learn every day from colleagues.
While this may seem like a common standard, continuous training, and management of in-house coders is a tedious time-consuming task to keep up with. Waiting to explore outsourcing the job to companies that specialize in end-to-end RCM medical coding does more harm than good.
3. Ensure HCC and SDOH are always on your radar
Deloitte4 found that an increase in value-based purchasing and at-risk payment models has heightened interest in improving the health of the populations being managed. Consequently, accurate coding for risk factors HCC Coding and SDOH capture has become more critical than ever. In 2021, providing quality care, reducing costs, and avoiding potential loss of revenue for healthcare providers means leaving every stone unturned for a comprehensive deep dive.
The Center for Medicare and Medicaid Services (CMS) mandates the use of Hierarchical Condition Categories (HCC) coding to calculate the reimbursement under Medicare.
HCC codes consider a patient’s demographic factors, such as gender, age, etc., and current health status to calculate a risk adjustment factor that determines the patient’s expected healthcare spending for the year.
HCC coding allows providers to receive adequate and fair compensation for treating patients with higher risk while providing value-based care.
Therefore, managers and leaders must ensure every stakeholder understands the impact of proper HCC coding on revenue cycle management. For example, physicians must document the patient’s condition to the highest levels of specificity using the M.E.A.T criteria, making it easier for coders to assign the correct codes.
Similarly, coding for the social determinants of health (SDOH) improves the patient care and experience, reducing readmissions, contributing to a healthy revenue cycle. SDOH are the socioeconomic factors in the environment where the patient lives, which can be grouped into five categories - (i) economic stability, (ii) education access and quality, (iii) healthcare access and quality, (iv) neighborhood and built environment, and (v) social and community context.
According to the 2021 regulations around SDOH, all clinicians, i.e., providers, case managers, social workers, nurses, etc., must collect data around social needs, including lack of food, homelessness, social isolation, etc. Coding managers must ensure coders are familiar with the use cases of SDOH Z codes and have the right support and encouragement to execute coding around social needs, which was previously assigned a lower priority.
4. Don’t skip the coding compliance audit.
Complete and accurate coding leads to a high-performing revenue cycle and ensures compliance with government healthcare regulations.
A Change Healthcare study5 found over $262 billion in claims were initially denied in a year primarily due to insufficient clinical information, with $28 billion in denied funds linked to lack of clinical documentation.
Ensuring medical coding practices are at par with the stated guidelines and procedures can prevent such denials that require additional information for reimbursement.
A coding compliance audit examines a specific number of charts per qualified healthcare professional to check the accuracy of the services documented and codes recorded.
Therefore, performing quality audits highlights areas of improvement that cause revenue leakage, identifies opportunities for training and workflow correction, and expedites claim reimbursement by reducing denials.
Upon the completion of the audit, providers must openly communicate the audit findings and arrange education and training programs, if necessary. Additionally, they must also communicate any changes in coding compliance, especially during unexpected and unprecedented situations like the COVID-19 pandemic that can potentially change revenue cycle coding processes.
How can ECLAT help?
It is imperative for healthcare providers to improve their bottom line by ensuring reimbursements are in order with the proper documentation and coding. Partnering with a coding solutions company, such as ECLAT Health Solutions is one way to assist providers with as-needed experienced services -- coding, coding education and audits.
ECLAT’s unique service delivery blend of domestic and global resources provides an affordable solution for any Revenue Cycle Management team looking to improve ROI.
As an end-to-end revenue cycle management strategies partner, ECLAT understands that efficient, accurate, and complete medical coding is crucial to maintain a high-performing revenue cycle.
Our AHIMA and AAPC-certified revenue cycle coders are experts in ICD-10, CPT4/HCPCS, MS-DRG, and more, delivering high-quality revenue coding services (95% or greater accuracy) and timely submission to payers.
Additionally, our 3-Tier Quality Assurance Process identifies and fixes any/all errors to minimize denied claims. As part of our offshore medical coding services, we offer a 24-hour turnaround time, along with weekend and holiday coverage at no additional cost, if required.
To learn more about our RCM medical coding services, please feel free to schedule a 1:1 consultation with our RCM experts.
References:
- HFMA.org
- Hospitals' claims denial rates rose to new heights during COVID-19, executives report
- BESLER and HIMSS Media Partner to Uncover Today's Hospital Revenue Cycle Vulnerabilities and Opportunities
- Social determinants of health: How are hospitals and health systems investing in and addressing social needs?
- Change Healthcare Analysis: An Estimated $262 Billion in Healthcare Claims Initially Denied in 2016

.jpg)
