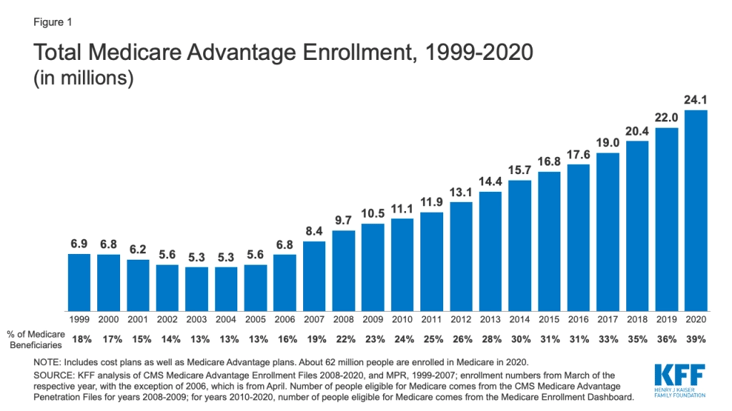
Medicare Advantage enrollment has doubled over the past decade1 and is projected to increase by 51 percent by 2030.
HCC coding is used by any healthcare provider that accepts Medicare Advantage plans. Coding and revenue cycle leadership at MA organizations are probably well aware that there is always a high chance that error or missed risk-adjusted reimbursement if HCCs are not carefully audited internally prior to the initial sampling period under the CMS-HCC model.
Having delivered HCC Coding Services to facilities and health systems across the nation, we realize the complexities involved in understanding how the 9,700 ICD-10-CM codes map to one or more of the 86 HCC codes.
Inaccurate reporting or erroneous capturing of HCC codes can affect patient Risk Adjustment Factor (RAF) scores resulting in:
- Missed reimbursement opportunities
- Non-compliance with CMS Guidelines
- Value-based healthcare inconsistencies
- RADV Appeals, and more
Consider following the below best practices to improve your organization’s HCC coding accuracy and maintain readiness for the annual Risk-Adjustment Data Validation (RADV) audits.
1. Address Specificity in Documentation using the M.E.A.T. Criteria
Risk adjustment and HCC coding relies on the abstraction of accurate and comprehensive documentation of chronic condition diagnoses by providers every year and combined for additive calculation. Providers need to verify that all the conditions of a patient are thoroughly assessed. In addition, the highest degree of specificity should be maintained during documentation. Remember, even the smallest differences in specificities can alter a patient’s treatment plans, code assignments, and RAF scores for predictive years.
Several healthcare organizations today implement policies that abide by the M.E.A.T criteria to ascertain the most accurate documentation for coding specificities.
This acronym stands for Monitoring, Evaluation, Assessment, Treatment which entails the following:
- Monitoring: signs, symptoms, disease progression, disease regression
- Evaluating: test results, medication effectiveness, response to treatment
- Assessing: ordered tests, discussion, review records, counseling
- Treating: medications, therapies, other modalities2
2. Facilitate Education For Your Physicians and Coding Staff
Physician documentation is key to HCC coding optimization. HCC Codes can only be optimized by increasing the level of specificity of the clinical documentation provided. Likewise, continuous ongoing education about HCC coding guidelines is essential for your coding team to apply the latest updated regulatory standards for high-quality scores. COVID-19 has also contributed to the added pressure physicians often feel when they are expected to focus on HCC coding regulatory upkeep in addition to the numerous responsibilities they already have on their plate.
Here are some tips for consideration as you navigate change management:
- Identify and engage physicians who can champion the importance of HCC coding among their peers.
- Identify the most commonly used and frequently occurring HCC codes in your organization and have physicians focus on them instead of all the 86 HCC categories.
- Provide and prioritize opportunities for education to elevate the importance of value-based contracts with cost-benefit scenarios that increase understanding of how HCC coding works, financially speaking. Sometimes, return on investment (ROI) can be the most effective motivation.
Provide regular training sessions to your coders so they stay up-to-date with these quarterly and annual updates and maintain compliance.
As part of our HCC coding Services, ECLAT Health Solutions provides education and training programs to your team. Stay vigilant for HCC codes concurrently if resources are available to reduce the time lag for upcoming reporting periods. Provide weekly or monthly mock audits with all participating parties and review the performance at the end of the mock audit so that changes based on the insights can be quickly implemented. All of this can help your organization avoid lost revenue opportunities prior to the reporting period.
This includes monitoring how provider education helped influence proper risk assessment for the future. It’s important to constantly monitor the success of your provider education program. Track KPIs including documentation completeness, reporting errors, claim denial rates, before and after the launch of the program. AHIMA also recommends that "Risk adjustment coding professionals should identify the documentation gaps and guide providers on how to eliminate the gaps"3
3. Make sure secondary diagnoses are reported properly
Lack of proper documentation and reporting of secondary diagnoses results in an incomplete picture of the patients and thereby becomes a common reason for loss of reimbursements. Pulling information from multiple data sources (hospital inpatient, hospital outpatient/ physician) can easily turn into missed opportunities for optimal reimbursement. Secondary and/or chronic conditions are often not reported especially in outpatient encounters. Part of this can be due to data interoperability, which is another important factor to take into consideration when reviewing the root cause of low-risk factor scores.
In order to overcome this, we usually advise and work with clients that are able to perform a secondary internal risk assessment review. This secondary review helps close the HCC documentation gaps that might have been missed in the primary risk assessment review.
4. Seek assistance from HCC Coding Experts sooner than later
Converting medical documentation into HCC codes is not as simple as it sounds. This tedious task requires specialized coding expertise and proficient experience with knowing where to search deeper for coding acuity, and raise awareness when needed. If you are not confident that you are reaping the benefits of optimal reimbursements, consider outsourcing certified risk adjustment coders who deliver consistent and compliant HCC coding performance. Partnering with a global HCC coding vendor helps release the administrative burden for providers sooner than later and allows them to focus on delivering better patient care.
The ECLAT medical coding and billing services team consists of credentialed AAPC and AHIMA coders who are specialized in coding services including HCC code assignment. We can help you feel confident about CMS Audit samples prior to submission deadlines to obtain optimal reimbursement. Learn more about our HCC coding services and witness the ECLAT advantage to optimize value-based reimbursement.
Why Consider ECLAT For Your HCC Coding Needs?
- We help you get ready for RADV audits by providing
- HCC coding education
- Assistance with physician queries
- Flexible staffing up to full-outsource capability.
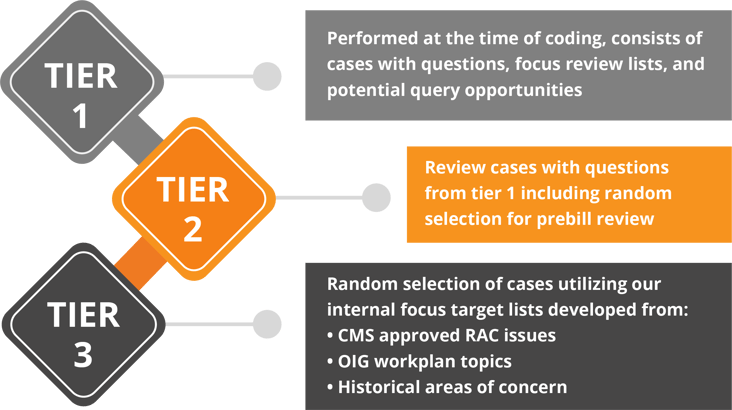
- You can achieve optimal RAF scores with our proprietary 3-Tier Quality Analysis process, which can be completed within a 24-Hour Turnaround Time (TAT).
For any questions regarding our Risk Adjustment services or HCC Coding availability for outsourcing, click here.
Reference:
1. Kaiser Family Foundation (KFF), 2020 report.
2. Source: American Academy of Professional Coders
3. AHIMA - Documentation and Coding Practices for Risk Adjustment and Hierarchical Condition Categories
4. CMS Report

.jpg)
